Back to "Normal": Why Hospitals Could See Millions of New Uninsured Patients this Year

You’ve probably heard that the Medicaid program will be facing some major changes this year. However, as with many government-mandated processes, it can be challenging for hospitals to understand what lies ahead for their patients and financial systems in 2023 and beyond.
Over the past few months, Congress has passed several pieces of legislation, and decisions have come out of Washington, D.C., that impact the immediate future of Medicaid. Here’s what you should know about the Medicaid redetermination process and how your organization can best prepare.
What’s happening?
One-sentence summary: Additional funding available during the public health emergency caused by the COVID-19 pandemic led to tremendous growth in Medicaid, but new legislation will suspend auto re-enrollment, likely leaving millions without coverage.
Medicaid enrollment has trended upward throughout the PHE
Since the start of the COVID-19 pandemic three years ago, Medicaid has seen a 27% growth in enrollment. In late 2022, nearly 91 million Americans were enrolled in Medicaid, about 19 million new people since early 2020.
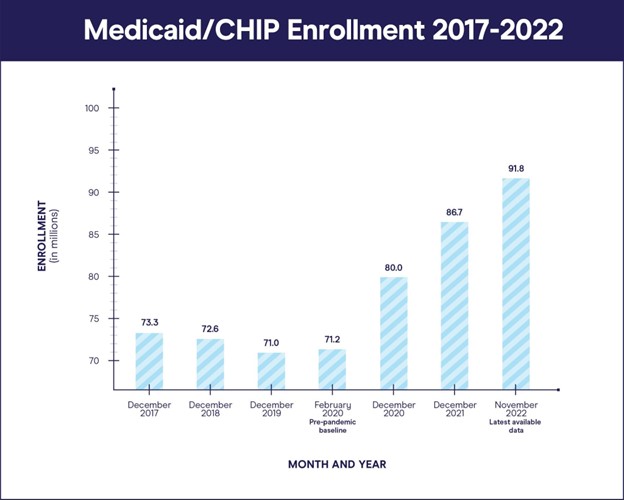
Source: Kaiser Family Foundation: https://www.kff.org/coronavirus-covid-19/issue-brief/analysis-of-recent-national-trends-in-medicaid-and-chip-enrollment/
For many, Medicaid fulfilled its purpose as a safety net meant to help Americans who lost their jobs or income as a result of the pandemic and subsequent public health emergency (PHE). Without it, hospitals would have seen explosive growth in uninsured patients, all while being overwhelmed with new COVID patients.
Under normal circumstances, there would be quite a bit of turnover in the number of people enrolled in Medicaid as eligibility expired for some people each month. But in these unique circumstances, Medicaid enrollment continued to grow over the past few years due to the enactment of the Families First Coronavirus Response Act (FFCRA).
Since March 2020, FFCRA has provided additional Medicaid funding to individual states on the condition they do not disenroll anyone from Medicaid. Without coverage expiring, anyone enrolled in Medicaid has remained active throughout the PHE.
The omnibus bill has effectively suspended the auto re-enrollment provision
The omnibus bill, passed in December 2022, has revoked this condition by delinking Medicaid from the PHE (which is set to expire in May of this year anyway). This means the Medicaid re-enrollment process will return to “normal” this year. States will gradually lose the extra funding provided by the FFCRA and will now need to continually evaluate and enroll Medicaid patients every 12 months.
This process has been given many names, including “returning to normal,” “unwinding” and “delinking.” We will refer to it here as “unwinding.” The unwinding process is managed by the state and may be different depending on where your hospital or health system is located.
Legislation passed via the omnibus bill set a specific date of April 1, 2023 as the day when states can begin the process of “unwinding.” Medicaid patients may be “disenrolled” from the program at this point, provided they have been given adequate notice.
What will be different moving forward?
One-sentence summary: As people must actively re-enroll to continue coverage, overall Medicaid enrollment will go down, leading to an influx of self-pay patients.
The number of people enrolled in Medicaid will shrink
Right now, the United States is experiencing a record low rate of uninsured patients, but the redetermination process will certainly cause this number to increase. Remember, Medicaid enrollment skyrocketed during this time, bringing an influx of new patients who have never navigated the traditional re-enrollment process and may not know where to start. It’s currently estimated that 8% of eligible patients will lose coverage during redetermination. That’s nearly 18 million people!
It’s also expected that redetermination is likely to disproportionately impact children, low-income households and people of color. In 2021, Black and Latino people made up around ⅓ of the total U.S. population, but about half of the total people enrolled in Medicaid and the Children's Health Insurance Program (CHIP). These populations are more likely to experience re-enrollment barriers like lack of knowledge, unstable living situations and tedious, paper-based systems, preventing easy re-enrollment.
States will start to lose additional funding over the next 12 months
As states lose their extra funding for Medicaid, there were early concerns they would have incentive to dis-enroll people from the program as quickly as possible as these patients are no longer being covered by federal funding. However, the Consolidated Appropriations Act, passed as part of the omnibus bill, provides for a gradual decrease in funding rather than an abrupt end.
Starting April 1, 2023, excess Medicaid funding will drop five percentage points. In the third quarter (starting July 1), it will drop 2.5 percentage points, then 1.5 percentage points in the last quarter of 2023. The Biden administration is encouraging states to take the entire, 14-month period provided for redetermination to give patients plenty of notice and time for instruction on how to remain enrolled and continue coverage uninterrupted.
More self-pay patients will receive care from your hospital
The bottom line is that ultimately your hospital or health system will see an increase of self-pay patients coming through your doors. This is an imminent concern as many organizations’ financials depend on Medicaid coverage as a significant source of income. It’s in your best interest and the patients’ best interest to keep eligible populations enrolled.
How can you prepare for Medicaid redetermination?
One sentence summary: Know your state’s plan and timeline for redetermination and remain proactive in assisting existing patients in the re-enrollment process.
Understand what your state is doing
It’s up to each state to determine its own plan and timeline for the coming “unwinding.” Coordination and timing will vary depending on your geographic location, but both the state and its hospitals and health systems have a vested interest in working together to help patients stay enrolled.
Keep an eye on your state’s Medicaid website and communications to understand their guidelines and approach and take these into consideration when planning your own strategy for handling redetermination. It’s also a good time to think about coordinating your efforts with your state’s Medicaid office for outreach and engagement actions explaining to patients how and why they must re-enroll.
Be proactive
It’s easier to assist a patient in the re-enrollment process than to have them come in for care and then assist them with an entirely new application. New applicants come with a higher cost and delayed reimbursement, so it’s best to be proactive and upfront in your efforts.
If they haven’t already, hospital revenue cycle leadership should start planning how they will reach out and engage with patients. Gathering knowledge on redetermination should remain a priority over the next few months as new legislation takes effect.
Luckily, the tools and partnerships you need to navigate the coming months exist and are available. Office Ally has been operating in the insurance verification and Medicaid eligibility and enrollment space for more than 20 years. We’re proud to serve as a trustworthy source of information and customizable software solutions to help you come out of this transition on top.
We’re here to help. Contact Office Ally today to connect with one of our experts for more information.







.svg)

.png)


.png)





