What is Medicaid Redetermination? | A Complete Guide to the Renewal Process | 2023 Update

Medicaid redetermination is the process of reviewing Medicaid eligibility for all enrollees to confirm they still qualify for the program following the end of the continuous enrollment provision. It officially began April 1, 2023.
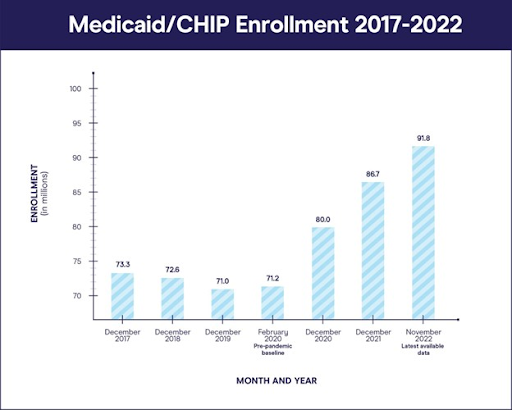
At the start of the COVID-19 pandemic, the U.S. government declared a public health emergency (PHE). Subsequent legislation (the Families First Coronavirus Response Act, or FFCRA) allowed for additional funding for Medicaid, provided each state refrained from disenrolling patients for any reason. Since then, Medicaid has seen a 27% growth in enrollment. In late 2022, nearly 91 million Americans were enrolled in Medicaid, about 19 million new people since early 2020.
Prior to the PHE, state-run Medicaid programs evaluated patients annually to ensure they still met requirements for qualification. These annual evaluations will resume after the unwinding process. States will gradually lose the extra funding provided by the FFCRA and will need to continually evaluate and enroll Medicaid patients.
This process has many names, including “returning to normal,” “unwinding” and “delinking.” We will refer to it here as “redetermination.”
How Medicaid enrollment works
Medicaid is a government healthcare program in the United States that provides medical assistance to low-income individuals and families, provided they meet certain qualifications. These key terms provide an overview of how the process usually works.
Typically, patients receive a renewal notice stating they will have to provide information for Medicaid coverage continuation. This notice outlines the specific Medicaid renewal requirements and the deadline for submitting the necessary renewal documentation.
During the Medicaid eligibility review, caseworkers or automated systems assess the provided documentation to verify that the recipients still meet the income and other eligibility criteria for renewal. If there are any changes in the recipient's circumstances that affect their eligibility, they may no longer qualify.
Prior to the PHE, the renewal process played a crucial role in program integrity by ensuring that Medicaid resources are appropriately allocated. By regularly evaluating eligibility, the program can efficiently manage resources and provide healthcare access to those who need it most. Ideally, Medicaid redetermination will return the system to this “normal” process.
What does redetermination mean for Medicaid?
The FFCRA has ensured anyone enrolled in Medicaid retained coverage throughout the PHE without fear of expiration. Because of this, Medicaid enrollment has trended upward over the past three years. The program has done its job as a metaphorical safety net for patients while preventing hospitals from experiencing a surge in uninsured accounts.
However, new legislation has revoked this condition and suspended auto-enrollment, which has prompted the redetermination process. States must work to re-enroll patients before they lose coverage.
It’s a big deal in the American healthcare system, which has never seen such a large-scale disruption. Early estimates show millions could lose coverage as a result of Medicaid “churn” brought about by redetermination.
Churn occurs when people fall out of Medicaid coverage for a short period of time but eventually re-enroll. It differs from a permanent loss of Medicaid coverage, which often occurs when a patient transitions off of Medicaid and moves onto a new coverage plan, like an employer-sponsored commercial insurance program.
One of the worst case scenarios surrounding Medicaid churn occurs when a patient does not re-enroll in Medicaid despite remaining eligible. That patient then loses coverage without transitioning to a new type of insurance, leading to a lapse in coverage (and often care) that lasts indefinitely.
Since the start of the COVID-19 pandemic three years ago, Medicaid has seen a 27% growth in enrollment. Patients who joined during this time have never experienced the renewal process, and likely will not know they have to renew at all, costing them their coverage.
It’s estimated that 15 million total people will lose Medicaid coverage through redetermination. Around 6.8 million will lose coverage despite remaining eligible.
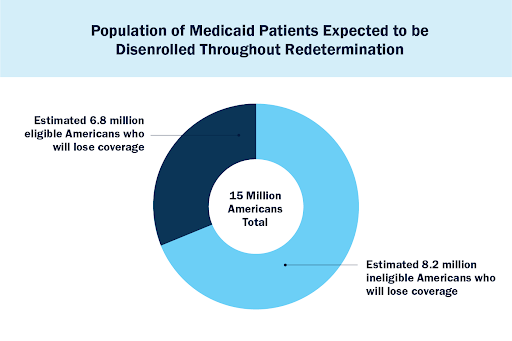
Projected Medicaid disenrollment pie graph: Expected reduction in Medicaid patients during redetermination
Many people who enrolled in Medicaid during the PHE have never re-enrolled. They may not know they have to re-enroll at all, or they may not understand the process. Some states still use complex, hard-to-navigate, paper-based systems. It’s also difficult to reach some patients to initiate the re-enrollment process due to unstable housing or communication situations. Without up-to-date addresses, it’s likely these patients will never receive paper-based communications at all.
The list of eligible Americans at risk of losing Medicaid coverage is not homogenous or limited to one demographic. However, research has uncovered a series of patterns that suggest our most vulnerable populations are the ones most at risk, including low-income populations, people of color, chronically ill populations and children.
Medicaid redetermination timeline
The Centers for Medicare and Medicaid Services (CMS) have provided a clear timeline of the unwinding process. The official Medicaid redetermination start date was April 1, 2023. CMS permitted states to begin notifying patients of redetermination and the new for renewal as of February 1, 2023. However, states could not legally disenroll patients until April, provided the patient received advance notice.
CMS also provided a list of strategy options for redetermination, giving states the freedom to choose how they would approach the process and prioritize patient accounts for outreach. The four strategy options are:
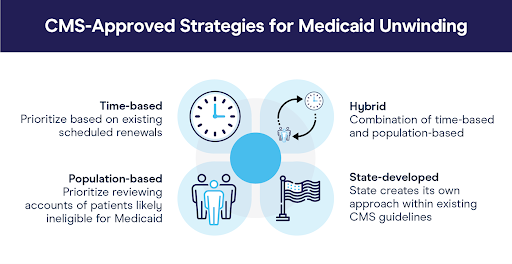
Following the release of CMS’s Medicaid redetermination guidelines, states began selecting their strategies and rolling them out. Four states began to disenroll Medicaid patients as of April: Oklahoma, Idaho, New Hampshire, and South Dakota. The majority of states (45) began disenrolling patients in May, June and July. The last state to begin redetermination is Oregon in October 2023.
The aftermath of Medicaid redetermination
While it’s still early in the process, there are some things we have already learned and others we can anticipate. For one, while initial estimates projected around 6.8 million people would lose coverage throughout redetermination despite remaining eligible, that number could increase.
This means that post-redetermination, the Medicaid population will definitely shrink. However, unlike during the PHE, every patient will have experienced the Medicaid renewal process and are invested in maintaining coverage. Hopefully, these patients will have a deeper understanding of the process and will emerge as more educated consumers.
Meanwhile, states will also have a better understanding of how to communicate with Medicaid populations after undergoing the work it takes to digest, process and funnel information from CMS to patients. States should also emerge better prepared for future emergency situations and disruptions that impact Medicaid lest one arises.
Ultimately, though the Medicaid redetermination process is complicated and bears heavy consequences, it also provides opportunities for patients and providers to come out ahead more educated, informed and prepared to maintain Medicaid coverage into the future.
As healthcare finance professionals, our job is to protect vulnerable populations and advocate for their continued Medicaid coverage.
Providers have a rare opportunity to leverage available tools and data that make redetermination much easier for both patients and staff. Download Office Ally’s free Medicaid Unwinding Playbook to learn more.







.svg)

.png)








