How to Prioritize Medicaid Patient Outreach During Redetermination

With Medicaid redetermination well underway, patients and providers alike are already experiencing the impacts. Initial estimates found around 6.8 million people were projected to lose coverage throughout redetermination despite remaining eligible - and that number could increase. Now, just a few months in, over 1.6 million eligible people have already been removed from the Medicaid system.
As we’ve previously covered, research has suggested these 6.8 million people are primarily vulnerable, at-risk populations, including children, low-income households and chronically ill patients. It makes both ethical and financial sense for providers to expend resources assisting these patients in maintaining coverage, which can feel like an overwhelming task.
However, by leveraging realtime Medicaid eligibility verification, retrospective lookbacks for recent changes in coverage and insurance discovery, you can better prioritize your workflow and understand which patients are on the verge of losing coverage. This will allow you to act quickly and prevent eligible patients from experiencing a lapse in coverage.
Step 1: Insurance Discovery
There are several sources of data you will be able to leverage to create the foundation for your prioritization strategy.
Patients may have lost coverage due to the ongoing redetermination process or they may have converted to active commercial insurance. By running your current patient population through the insurance discovery process, you will end up with a list that separates patients by:
For prioritization purposes, the following steps will focus on patients in category 1 who have active Medicaid coverage, and patients in category three, who have lost coverage but remain eligible.
Step 2: Cross-reference clinical information
From there, cross-reference patients with active Medicaid coverage by existing clinical information. What care have you provided these Medicaid patients with over the past 1-3 years? There are two categories of patients we recommend flagging:
Patients in these two categories who are actively enrolled in Medicaid or have lost coverage despite remaining eligible should be at the top of your prioritization list. From here, you can move into the outreach process.
Note: Providers in New York, Arizona and Tennessee are able to get an additional dataset of Medicaid expiration dates for their patients. If possible, we recommend obtaining this data to help prioritize by date in addition to the above criteria. Hopefully more states will offer this data in the near future!
Step 3: Develop a proactive outreach strategy
Next, hospitals can proactively outreach to these VIPs (Very Important Patients) and make sure they are aware of two things. One, that their coverage must be renewed this year and two, that you are a valuable resource to help them through this process.
We suggest creating a comprehensive strategy that includes both direct outreach and outreach via electronic, automated tools.
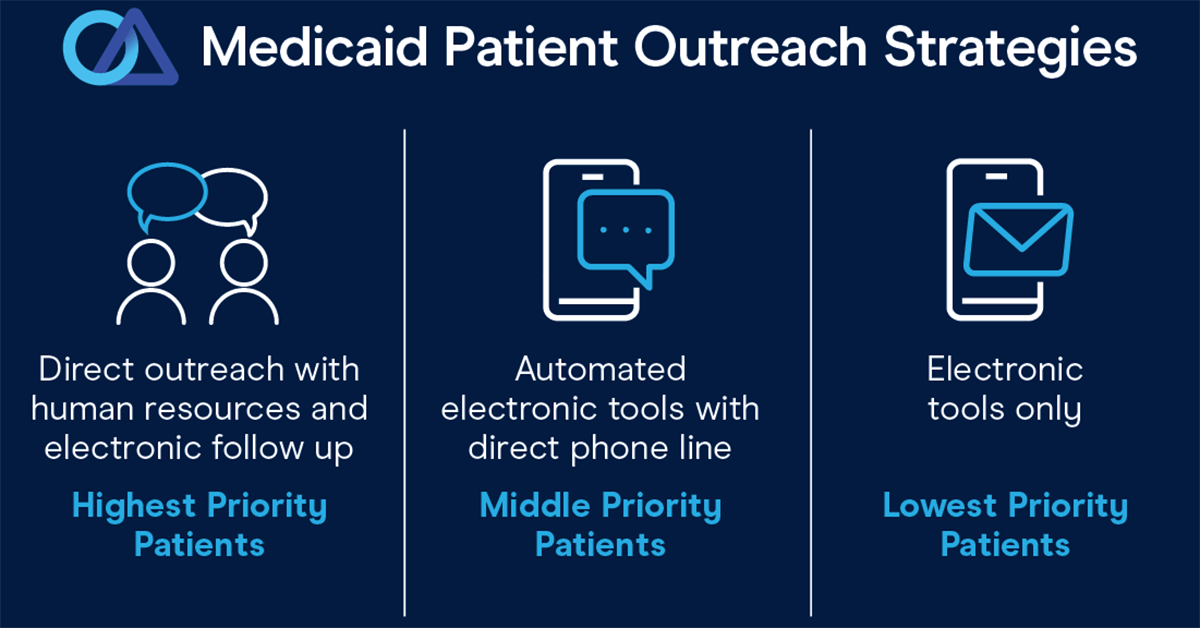
Direct outreach, which requires human resources, should be reserved for the patients identified in Step 2. Providers can call directly, but they can also leverage digital tools, like texting, email, patient portals and other electronic communication to engage with these patients to make sure they won’t lose coverage or, if they already have lost coverage from redetermination, get them re-enrolled as quickly as possible before they require any further care.
These same tools can be used to integrate outreach with the pre-registration process. Hospitals can send appointment reminder texts and emails with an extra note for Medicaid patients urging them to check their eligibility and prepare to re-enroll.
For Medicaid patients who are not frequent visitors to the hospital or who do not have an upcoming appointment, automated electronic tools can be extremely useful as they require limited human time and resources. Medicaid patients can receive texts, emails or patient portal notifications on an automated timeline driving them to information on their state’s redetermination process with a phone number or email they can contact if they need assistance from the hospital to re-enroll.
This three-step process allows patient financial services to prioritize accounts by identifying those most likely to qualify for enrollment or re-enrollment into a reimbursement or patient assistance program, such as Medicaid. Leadership can then define their outreach and engagement flow based on these scores, integrating high touch procedures for priority accounts and more automated, email-based procedures for remaining accounts.
Useful tools for prioritization and outreach
There are a wide variety of trusted data sources that can be used to assist financial counselors in assessing patients' financial situation. A best practice is to use multiple tools and deploy them in a manner that is consistent with organizational policies.
Luckily, the tools and partnerships you need to navigate the coming months exist and are available. Office Ally has been operating in the insurance verification and Medicaid eligibility and enrollment space for more than 20 years. We’re proud to serve as a trustworthy source of information and customizable software solutions to help you come out of this transition on top.
We offer the following software tools to assist in patient prioritization:
There is little to no precedent for the current Medicaid unwinding in the American healthcare system. When you and your team are in uncharted waters, the right software tools can make all the difference in successful navigation.
It’s not too late - now is the time to design a customizable system that caters to your existing needs and processes while preparing your team for a swift, successful Medicaid unwinding in 2023.







.svg)

.png)








